Overview
This project was developed as a product and implemented for a fully accredited RCM company in the Midwest with over 30 years’ experience in medical reimbursement management. The Minnesota-based firm provides medical billing, coding, credentialing, and consulting services for multi-specialty medical professionals.
Challenge
Accurate eligibility verification is a critical factor in the claims submission and reimbursement process. The rising work volume the team was handling through manual processes was strikingly undermining the efficiency. The team was verifying the eligibility of about 1000 patients daily for the upcoming appointments by logging into the provider portaland cross-verifying it from carrier portal. The data from the client application and extracted data from the provider portal is updated into the front-office application and eligibility report is generated.

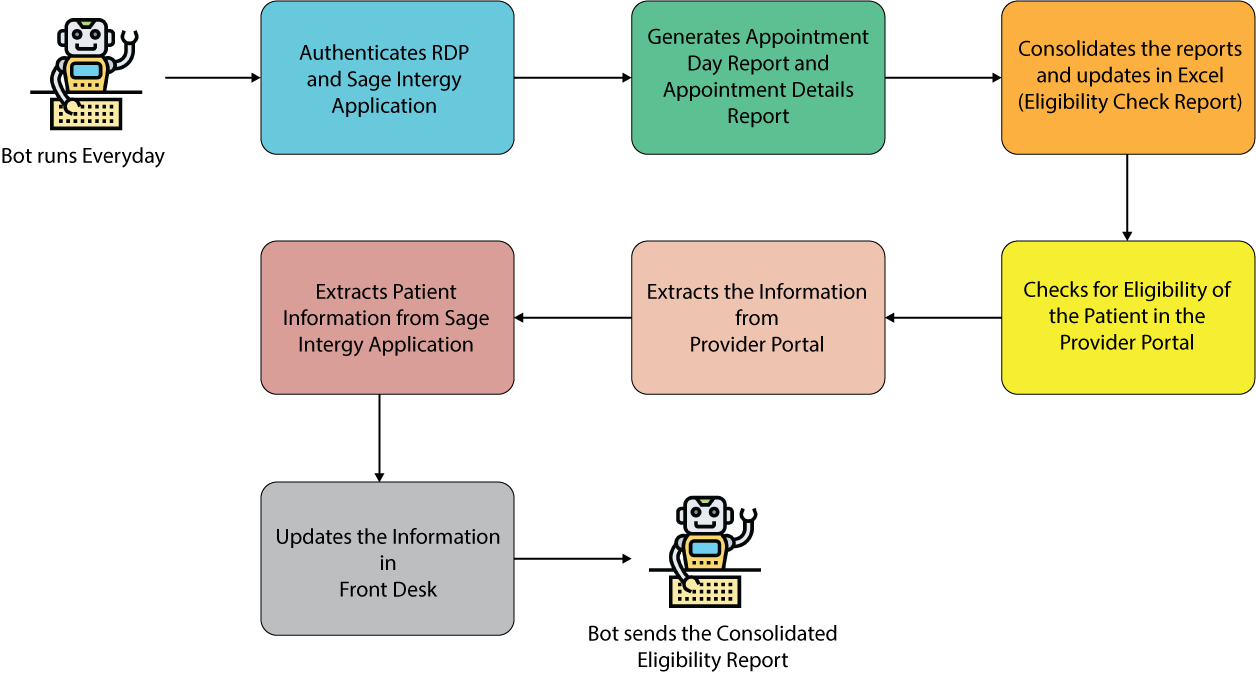
Our RPA team built an intelligent robot that ran for 15 hours 7 days a week to execute the process through the following apps.
- Provider application authentication: Bot authenticates provider application and extracts appointment details for all patients.
- Export Appointment Details reports to Excel: Bot copies appointment details of the last 24 hours to the corresponding template and filters the unwanted data.
- Generate Eligibility Check report: The data is then copied to the eligibility check report template.
- Check eligibility: It then consolidates the reports, validates the eligibility, extracts patient information from the provider portal, and updates the front-office web portal for respective patients. The details updated in the portal include patient name, insurance term, guarantor due, and the eligibility check report is updated.
- Task notification: A process status email is sent to the team as specified in the configuration file.
- Real-time eligibility and benefits verification - Shortened patient check-in process
- Easy-to-read statements with co-pay and deductible details – Better informed patients and Quicker reimbursement for providers
- Elimination of repetitive manual tasks – Better utilization of resources
- High accuracy – Reduced errors, minimal unforeseen costs
- High efficiency – Reduced operating costs and staffing issues (1 bot can handle the workload of 4-5 individuals)
- Increment in Referrals due to improved patient experience
| Pre RPA | Post RPA | |
|---|---|---|
| Transactions per day | 1000 | 5000 |
| Accuracy rate | 63% | 97% |
| Headcount | 10 | 1 |
*25% cost savings for the organization within the first year
*Besides operational efficiency, there has been a marked increase in patient satisfaction.
Technology Stack
- UiPath
- Sage Intergy Application
- Front-office web portal
Speak to our Experts!
Countless businesses around the world and across industries have gained substantially from smart RPA implementations. Over the last decade, we have enabled our clients to transform their business by tapping their true potential with RPA. We can help you do that too!