The Stumbling Block Burning the Midnight Oil
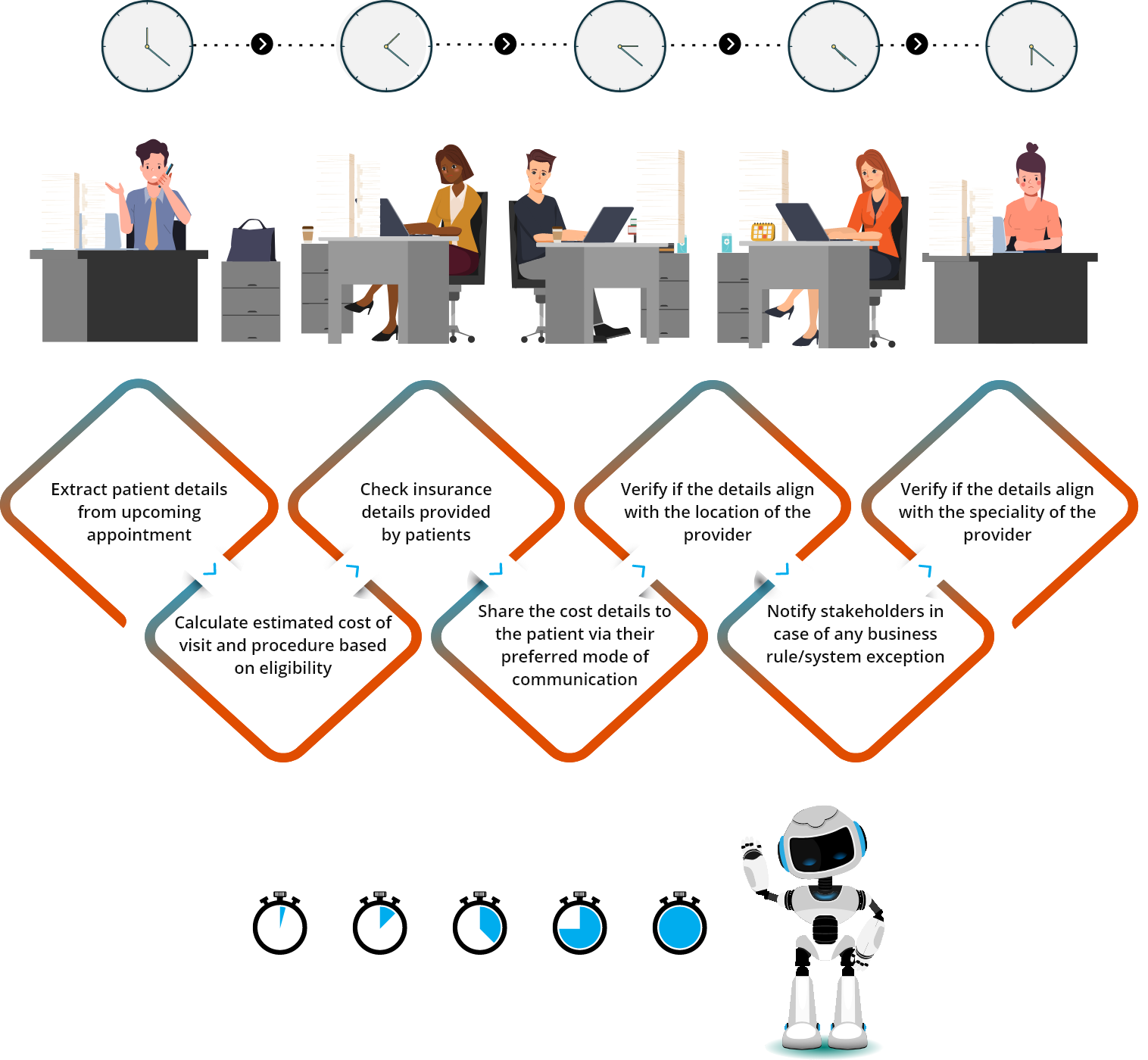
At a provider’s office, Michael, Pam, Ryan, Jim, and Mindy are huddled over their desks trying to manually verify a patient’s insurance eligibility status. Michael and his team offer advanced urology services in Georgia, USA. They perform urology-related surgeries, lab work, and testing, all in one facility.
Michael’s team verifies eligibility for each patient’s coverage and benefits before the patient’s visit. Pam and Ryan are focused on checking the insurance details provided by the patients and verifying them against the specialty of the provider. Jim and Mindy are involved in calculating the estimated cost of a patient’s visit and procedure and share the same with the patient via their preferred mode of communication. Michael manages the team and notifies the stakeholders if any anomalies arise.
Why is Eligibility Verification Needed?
Eligibility verification is done to avoid claim re-submissions, eligibility-related denials, lack of upfront collection, and so on. It all culminates in a smoother medical billing process and improved patient satisfaction.
However, Michaels’ team was always exhausted by the end of the day. The teams spent at least 13 minutes on average verifying the eligibility of one patient. Putting this into perspective, Michael’s team had to manually verify the eligibility of 1000 – 2000 patients in a day, at times. That’s an average of 13000 minutes, which is 216 hours. However, a day has only 24 hours, which made it impossible to manually verify the eligibility of every patient when the volumes were high as 1000 verifications a day.
When the eligibility of a patient is not verified, the care is delayed which results in poor health outcomes, reduced patient satisfaction, and ultimately a low Net Promoter Score.

The Savior – RPA bots
Michael noticed his team was struggling to meet the expectations and their patients were getting impatient with the delay. He remembered reading about automating healthcare workflows and decided to do some research on the same. Upon completing thorough research, Michael knew enough about Nalashaa’s expertise in the healthcare domain and decided to approach them for eligibility verification automation.
The team at Nalashaa instantly knew that this was where RPA implementation services and expertise would come into play. Before implementing the RPA bots, the team at Nalashaa did a thorough review of how Jim, Mindy, Pam, and Ryan executed the eligibility process.

Once the team at Nalashaa had clarity into the operations of Michael’s team, they outlined the processes that need to be automated. Once the necessary business rules and verification steps were fed into the RPA, the bot performed the following activities on a pre-determined schedule:
- Extracted patient details from their upcoming appointment
- Captured the insurance details from insurance plan’s portal for each patient - Co-pay, Coinsurance, Deductible, OOP, and network status of the patient
- Estimated the patient visit’s cost based on the service charge and eligibility information
- Communicated the patient cost for their upcoming visit with the estimated cost
- Notified internal stakeholders of any business rule and system exception
Turning Over a New Leaf
With over 98% of manual tasks reduced, Michael, Pam, Ryan, Jim, and Mindy were overflowing with gratitude and joy – they no longer had to sit for hours on end to carry out this painful process.
Michael’s team was not the only one who was happy about the RPA implementation. Michael’s bosses were all happy too. Automating the eligibility of verification enabled the clinic to accommodate more patients than before, helping them increase their revenue by 5%. With the RPA thoroughly screening for business rule/system exception, there was also a decline in the number of incomplete and non-payment by 20%.
All this boiled down to patients receiving care on time, better health outcomes, improvement in patient satisfaction scores, and ultimately a higher Net Promoter Score.
in revenue
on time
health outcomes
patient satisfaction
Promoter Score
Credit where Credit is Due
While eliminating manual tasks and automating the eligibility verification process to enhance efficiency, Michael's team had helpers outside of Nalashaa’s engineering team. Here are the software tools that helped the engineering team at Nalashaa to implement RPA.

UI Path Studio

MS Excel

MS Outlook

MS Excel VBA